From Agents to Case Managers: The Call Center Workforce of 2030
Healthcare call centers won't scale by hiring more agents. By 2030, AI handles the routine so humans can do what actually matters: resolve the hard stuff.
For decades, healthcare call centers have been built around one core assumption: more calls means more agents. Volume in → labor out. But as AI accelerates across patient access, triage, billing, and care coordination, that equation is breaking. The winning models of 2030 won’t scale through staffing alone — they’ll scale through workflow intelligence.
And that shift is transforming the role of the call center worker itself.
The End of the “Answering Phones” Job
Today’s agents spend a significant share of their day on tasks that are:
- Routine (insurance verification, benefit explanation)
- Repetitive (status checks, referrals, scheduling)
- Navigational (routing patients or coordinating clinics)
- Administrative (documentation + data entry)
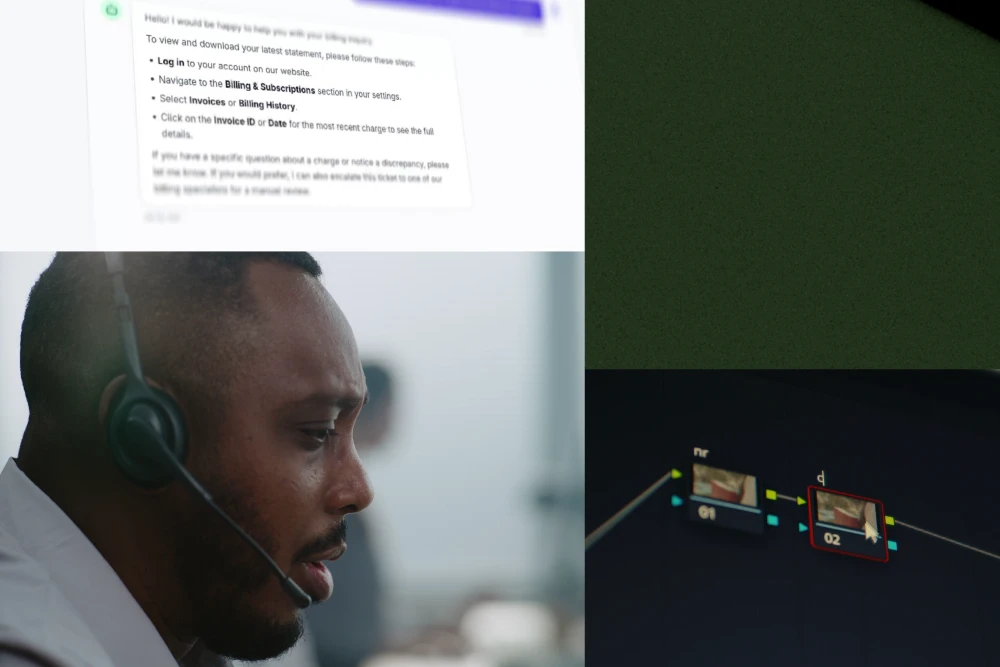
AI isn’t threatening to eliminate these tasks — it’s eliminating the friction around them:
- Conversational intake
- Eligibility lookups
- Benefit explanations
- Digital scheduling
- Documentation summaries
- QA & compliance auditing
- Predictive staffing
- Automated callbacks & follow-ups
Once routine work becomes automated or AI-assisted, humans move to what they’re uniquely good at: judgment, empathy, escalation, and resolution.
The New Role: Case Manager, Not Call Taker
By 2030, the frontline job in healthcare call centers is more likely to resemble a case manager than a call receiver.
What does that mean in practice?
Case managers will:
✓ Manage multi-step patient journeys (not one-off calls)
✓ Resolve complex situations that AI can’t auto-complete
✓ Coordinate between payers, clinics, providers, and families
✓ Navigate exceptions rather than standard workflows
✓ Apply clinical or operational judgment at key decisions
In other words: AI handles the repeatable. Humans handle the complex.
The Workforce Shift Is Already Starting
Forward operators are updating job ladders and training paths around the new division of labor:
Agents → Senior Agents → Case Managers → Care Navigators
This unifies what previously happened in fragmented silos:
- Patient access
- Billing inquiries
- Referral coordination
- Prior authorizations
- Clinical triage inputs
- Scheduling & rescheduling
- Follow-ups & outbound outreach
The value isn’t in answering the phone faster — it’s in navigating the system on behalf of patients with less leakage, fewer delays, and higher completion rates.
What This Means for Healthcare COOs Today
To enable this shift, operators will need to redesign four things:
1. Training & Competency Models
Training moves from scripts → decision trees → judgment frameworks.
2. Performance Metrics
Metrics shift from AHT (handle time) to resolution & completion rates:
- % of intents resolved
- % of cases completed
- Authorization throughput
- Referral closure rates
- Rework and leakage reduction
3. Organizational Structure
Hybrid teams grow that blend:
- Access
- RCM
- Care coordination
- Clinical input
Work becomes interdisciplinary, not siloed.
4. Technology & Workflow Integration
The tech stack evolves from telephony-first to workflow-first:
- AI intake + routing
- AI co-pilots for agents
- Automated documentation
- Integrated scheduling
- Real-time eligibility + auth workflows
- Case management platforms
The future is not about “having a call center” - it’s about managing patient access as a continuum.
The Upside: Better Work, Better Outcomes
This shift unlocks three major benefits:
For patients: faster access, fewer handoffs, less confusion
For staff: higher-skill work, less repetitive burnout
For operators: better economics + throughput without linear hiring curves
Healthcare access has been constrained by humans doing tasks that machines are simply better at. Once that weight is lifted, humans finally get to do the work that creates impact.
2030 Isn’t Far — It’s Just Operationally Uneven
The tech required for this model already exists. The difference between organizations who make the jump and those who don’t won’t be technological — it will be operational:
Do we redesign workflows around AI,
or do we bolt AI onto legacy workflows?
Healthcare operators who bet on the former will see the future arrive earlier.